Why You Should Avoid Tap Water in Your Neti Pot
 As spring unfolds, bringing vibrant blooms, millions prepare to face the challenges of allergy season, marked by sneezing, wheezing, and unyielding nasal congestion. Many people seek relief through the use of neti pots, which provide a drug-free solution by flushing out pollen and mucus with a saline rinse. However, studies indicate that tap water, when used in neti pots, may harbor organisms capable of causing rare, yet frequently fatal infections if not used correctly for nasal rinsing.
As spring unfolds, bringing vibrant blooms, millions prepare to face the challenges of allergy season, marked by sneezing, wheezing, and unyielding nasal congestion. Many people seek relief through the use of neti pots, which provide a drug-free solution by flushing out pollen and mucus with a saline rinse. However, studies indicate that tap water, when used in neti pots, may harbor organisms capable of causing rare, yet frequently fatal infections if not used correctly for nasal rinsing.
Neti pots are devices intended to clear out mucus and debris from the nasal passages using water. They are commonly used to relieve symptoms from nasal allergies, sinus problems, irritation from dry air, or colds. However, recent studies by the U.S. Centers for Disease Control and Prevention (CDC) have highlighted that using tap water in these pots for nasal rinsing can heighten the risk of acquiring rare yet severe infections caused by Acanthamoeba, tiny organisms that are prevalent in soil, water, and air.
These single-celled creatures can lead to various symptoms and are fatal in 82% of cases, although infections are uncommon, impacting only 3-12 people in the United States each year. Despite widespread exposure to Acanthamoeba, the number of people who actually fall ill remains low.
Acanthamoeba is responsible for several serious health conditions, including:
Acanthamoeba keratitis- an eye infection that threatens permanent vision loss, particularly in individuals who wear contact lenses.
Granulomatous amebic encephalitis- a severe infection of the brain and spinal cord that occurs in immunocompromised patients.
Disseminated infection- a pervasive infection that affects the skin, sinuses, lungs, and other organs, predominantly found in those with weakened immune systems.
The research focused on 10 immunocompromised patients with conditions such as HIV/AIDS, cancer or kidney disease, who had utilized neti pots and later developed Acanthamoeba infections. Seven of these patients survived, likely aided by the early intervention for concurrent sinus infections. Infections by Acanthamoeba, particularly those impacting the brain or central nervous system, are challenging to treat effectively. Unfortunately, most cases involving brain infections typically lead to death.
Nasal irrigation tools like neti pots, squeeze bottles, bulb syringes, and battery-operated water devices are deemed safe and effective when correctly maintained and used. However, the agency advises against using tap water for nasal rinsing, even though it’s safe for drinking. This is because stomach acid can neutralize microorganisms such as bacteria, amoebas and protozoa found in low quantities in tap water, but these can survive in the nasal passages and lead to severe infections. For nasal irrigation, it is recommended to use distilled or sterile water, boiling tap water for 3-5 minutes then cooled, or water filtered through a device capable of removing infectious organisms.
To minimize the risk of waterborne infections, it is essential to use uncontaminated water and also to maintain good hygiene practices. This includes washing your hands thoroughly, keeping the neti pot clean and dry, and adhering to the manufacturer’s guidelines for use.
To view the original scientific study click below:
Acanthamoeba Infection and Nasal Rinsing, United States, 1994–2022



 Is it possible that items meant to ensure our safety are instead compromising our neurological well-being? Recent findings indicate that typical household chemicals, including those in flame retardants and disinfectants, may be to blame. Scientists have examined thousands of chemicals considered potentially dangerous, identifying two particular types as detrimental to brain cells. With neurological disorders impacting millions, and the incidence rate climbing, genetic reasons account for only a small portion of these cases. Thus, hinting at the significant role environmental influences play in their prevalence.
Is it possible that items meant to ensure our safety are instead compromising our neurological well-being? Recent findings indicate that typical household chemicals, including those in flame retardants and disinfectants, may be to blame. Scientists have examined thousands of chemicals considered potentially dangerous, identifying two particular types as detrimental to brain cells. With neurological disorders impacting millions, and the incidence rate climbing, genetic reasons account for only a small portion of these cases. Thus, hinting at the significant role environmental influences play in their prevalence. Recent research featured in Nature Metabolism indicates that dietary protein, especially a specific amino acid, significantly contributes to atherosclerosis. This disease leads to the buildup of plaques along the walls of arteries, triggering heart attacks and strokes, and accounts for a quarter of all fatalities worldwide.
Recent research featured in Nature Metabolism indicates that dietary protein, especially a specific amino acid, significantly contributes to atherosclerosis. This disease leads to the buildup of plaques along the walls of arteries, triggering heart attacks and strokes, and accounts for a quarter of all fatalities worldwide. Recent studies have highlighted the promising health advantages of trigonelline, a naturally occurring molecule present in coffee, fenugreek, and within humans. This breakthrough is crucial in advancing muscle wellness and performance, particularly in addressing the challenge of sarcopenia. It was found by a global team of researchers that individuals experiencing sarcopenia in their advanced years show reduced concentrations of trigonelline.
Recent studies have highlighted the promising health advantages of trigonelline, a naturally occurring molecule present in coffee, fenugreek, and within humans. This breakthrough is crucial in advancing muscle wellness and performance, particularly in addressing the challenge of sarcopenia. It was found by a global team of researchers that individuals experiencing sarcopenia in their advanced years show reduced concentrations of trigonelline. For those facing challenges with sleep quality, conventional advice often revolves around evening habits. However, emerging research suggests a more impactful approach rooted in daytime physical activity. According to a new study, altering one’s daily routine to include more exercise can play a vital role in improving sleep at night.
For those facing challenges with sleep quality, conventional advice often revolves around evening habits. However, emerging research suggests a more impactful approach rooted in daytime physical activity. According to a new study, altering one’s daily routine to include more exercise can play a vital role in improving sleep at night. The authors of a new study published in the esteemed BMJ journal highlight a significant gap in research on the health impacts of ultra-processed food. They point out that despite extensive discussion on the topic, there hasn’t been a thorough umbrella review that synthesizes and evaluates the collective findings of meta-analyses on this issue. To address this shortfall, they examined 45 meta-analyses, encompassing nearly 10 million participants, offering a comprehensive overview of the evidence on the health effects of ultra-processed food.
The authors of a new study published in the esteemed BMJ journal highlight a significant gap in research on the health impacts of ultra-processed food. They point out that despite extensive discussion on the topic, there hasn’t been a thorough umbrella review that synthesizes and evaluates the collective findings of meta-analyses on this issue. To address this shortfall, they examined 45 meta-analyses, encompassing nearly 10 million participants, offering a comprehensive overview of the evidence on the health effects of ultra-processed food. If you often find yourself browsing through the food aisles of grocery stores, meticulously reading labels and finding unfamiliar ingredients, then you may have come across a range of substances produced using nanotechnology. It is a groundbreaking field that has revolutionized the manufacturing of numerous everyday products.
If you often find yourself browsing through the food aisles of grocery stores, meticulously reading labels and finding unfamiliar ingredients, then you may have come across a range of substances produced using nanotechnology. It is a groundbreaking field that has revolutionized the manufacturing of numerous everyday products. The link between diet and overall well-being is well-acknowledged, yet understanding the exact impact of specific dietary choices on health can be challenging. The effects of food on brain function are particularly intricate, with ongoing research aimed at determining which diets best enhance cognitive abilities and brain health. In one investigation, researchers explored four different dietary patterns, concluding that a diverse and balanced diet offers the greatest benefits for brain health.
The link between diet and overall well-being is well-acknowledged, yet understanding the exact impact of specific dietary choices on health can be challenging. The effects of food on brain function are particularly intricate, with ongoing research aimed at determining which diets best enhance cognitive abilities and brain health. In one investigation, researchers explored four different dietary patterns, concluding that a diverse and balanced diet offers the greatest benefits for brain health.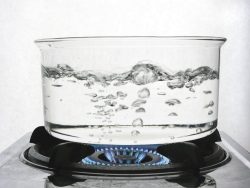 Recent findings from a study suggest that merely five minutes of boiling water could slash the concentration of microplastics in tap water by as much as 90%. Boiling tap water does more than just neutralize potential pathogens; it’s also effective in breaking down harmful pollutants like microplastics and chemicals, thereby enhancing the safety of your drinking water.
Recent findings from a study suggest that merely five minutes of boiling water could slash the concentration of microplastics in tap water by as much as 90%. Boiling tap water does more than just neutralize potential pathogens; it’s also effective in breaking down harmful pollutants like microplastics and chemicals, thereby enhancing the safety of your drinking water. A recent study has found a significant connection between the overconsumption of sweetened beverages and an increased likelihood of developing atrial fibrillation (AF), an irregular heartbeat condition. This condition can lead to serious complications, including blood clots, heart failure, stroke, and other cardiovascular problems. The research analyzed the genetic information and 24-hour dietary intake of over 200,000 participants, uncovering a clear link between sugary drink intake and the risk of atrial fibrillation.
A recent study has found a significant connection between the overconsumption of sweetened beverages and an increased likelihood of developing atrial fibrillation (AF), an irregular heartbeat condition. This condition can lead to serious complications, including blood clots, heart failure, stroke, and other cardiovascular problems. The research analyzed the genetic information and 24-hour dietary intake of over 200,000 participants, uncovering a clear link between sugary drink intake and the risk of atrial fibrillation.