Stem Cell Clinics in the United States

There are now more than 500 stem cell clinics in the United States and the FDA has been holding hearings to decide if they should be closed down or much more strictly regulated. The move comes at an awkward time because research on stem cell treatments is just starting to bear fruit. Tantalizing results from a series of small studies suggest injections with certain types of stem cells may be effective treatments for conditions such as stroke and multiple sclerosis. Also thousands of patients have been able to avoid joint surgery after receiving injections with stem cells and platelet rich plasma. Since Medical Doctors in Stem Cell Clinics generally use cells they?ve isolated from a patient?s own fat, and because those cells are considered only ?minimally manipulated,? the FDA has not regulated the treatments as it would a traditional pharmaceutical.
Patients who want immediate treatment for their conditions and Doctors who perform these treatments say the FDA is being pressured into taking a tough line by academics and pharmaceutical giants who want to control, and profit from, the stem cell industry.
?The problem is, if we do well, it hurts their business plan,? said Dr. Mark Berman, a plastic surgeon in Beverly Hills, California.
Back in 2002, Dr. Berman cofounded a chain of clinics called the Cell Surgical Network. He says he and other physicians in the network have conducted some 5,000 stem cell treatments including on himself and his wife for conditions such as arthritis and hip, back and joint pain. He called the draft regulations arbitrary and hypocritical.
The fight over regulation comes at a time when leading stem cell researchers, after years of disappointing results, are increasingly excited about new studies showing the cells appear to be safe and may be effective in treating a variety of crippling diseases, including macular degeneration and Parkinson?s.
?It?s a very exciting time,? said Sally Temple, a stem cell researcher at the Neural Stem Cell Institute in Rensselaer, N.Y. ?We?re going to see many treatments for diseases that are currently untreatable.?
The results researchers are so excited about are only possible because of decades of tedious work to establish safety protocols, test concepts and learn how to grow, produce, and manipulate stem cells, she said.
?It?s hard to have people understand how long this whole process takes,? said Temple, who also serves as president of the International Society of Stem Cell Research. ?You would not believe what we have to do in my lab to prepare cells properly.?
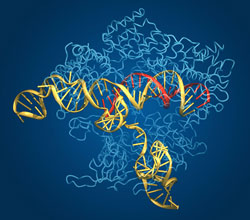
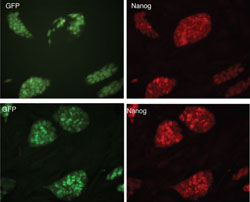
Stem cells can be extracted from a number of different tissues. They?re highly flexible and can turn into other kinds of cells ? heart cells, say, or retinal cells. That ability lets them act as a kind of internal repair system.
Stem cells extracted from bone marrow have long been used to treat cancer, and blood and immune disorders. Now a variety of types of stem cells are being tested in a slew of other applications.
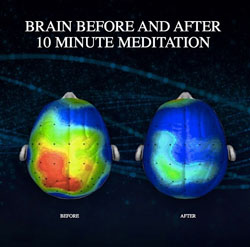
For example, a team at Stanford and the University of Pittsburgh announced in June in the journal Stroke that they had restored mobility in some stroke patients by injecting a particular kind of modified stem cell directly into their brains. Most stroke patients don?t improve much after six months, but some who received the treatment gained mobility a year or more after their strokes. Some who had been confined to wheelchairs even began to walk.
Dr. Gary Steinberg, a neurosurgeon at Stanford and the study?s lead author, said he thought the cells might be helping by secreting factors that led to the regeneration or reactivation of patient?s cells. ?We didn?t imagine we could restore neurologic function in these chronic stroke patients with severe disability,? said Steinberg.
The study just 18 patients; so Dr. Steinberg is recruiting 156 more for an additional study.
In another promising effort, a team from the University of Southern California announced they had restored some mobility in a 21-year-old man, Kris Boesen, who had become paralyzed from the neck down after a car accident this spring.
The team, led by USC neurosurgeon and bioengineer Dr. Charles Liu, injected 10 million specialized cells created from embryonic stem cells directly into the patient?s spine.
To be sure, it?s unclear whether, or how much, the treatment helped; the patient may also have recovered spontaneously. But whatever the mechanism, the improvement was dramatic: Three months after the treatment, the patient was feeding himself, hugging his family, and using his cell phone.
?The first thing he did when he could use his hands was text his girlfriend,? Liu said.
This patient was one of five enrolled in a multicenter clinical trial using cells that support nervous system functioning created from embryonic cells by Asterias Biotherapeutics, which plans to release results from several other patients Wednesday at an International Spinal Cord Society meeting in Vienna.
?If it bears out, it?s going to be huge,? Liu said. ?This was the difference between someone using his hands or not.?