It Isn’t All In The Genes – Are We Inheriting More Than We Think?
 Scientists have made a groundbreaking discovery about the mechanisms of healthy development in embryos, which could change our understanding on what we inherit from parents and how they shape us. The new research suggests that mothers may be passing on more of their DNA than we thought, with an epigenetic legacy for future generations.
Scientists have made a groundbreaking discovery about the mechanisms of healthy development in embryos, which could change our understanding on what we inherit from parents and how they shape us. The new research suggests that mothers may be passing on more of their DNA than we thought, with an epigenetic legacy for future generations.
It’s a recently discovered phenomenon called “epi-genetics”. The study, led by researchers from WEHI in Melbourne, Australia has significantly broadened our understanding of which genes have information passed down through generations and what proteins control this unusual process.
We all know that our genetics determine who we are, but what if there were other factors involved? DNA contains the instructions for producing all cells in your body. It’s really hard to change yourself and pass on these new changes because they happen through alterations of chromatin structure around genes which cause them not to be read by protein-coding regions any longer – so no products get made! This means you can have different versions or “epigenes” depending how much nutrition improves during development.
And it turns out that mothers can pass on their genes through epigenetics to a tiny extent. This means we need more research into how this works and what other factors come in play when determining whether or not an individual will have certain traits based off the DNA they’ve been given at birth. The new research has shown that a mother’s supply of protein can affect the genes which drive skeletal patterning in their offspring.
The discovery that mother’s DNA contains information passed on through generations has a deep impact on how we view ourselves. With this new understanding, there are many more questions than answers about what other types of environmental factors can affect our development and future health risks.
Researchers have recently discovered a new link between the mother’s eggs and her developing baby. This study focused on one protein, SMCHD1; it was found by Professor Blewitt back in 2008! The researchers wanted to see what would happen if they decreased or increased this level within an ovo- fertilized embryo before birth via maternal transfer. They monitored how many different types of Hox genes were activated throughout development as well because these play important roles during patterning for elegant structural formation.
It has been shown that mothers pass on their epigenetic information, rather than just the blueprint of genes. This is fascinating knowledge that we can now put to use. While there are more than 20,000 genes in our genome-the average human possesses around 150 of these coding regions which carry genetic information produced by mutation or choice over time. “This is the first time that we’ve seen this type of inheritance happen in human beings,” said Dr. Benetti, “and it gives us an idea about how few genes really matter over long periods.”
Research has shown that a gene called SMCHD1, which only exists in the fertilized egg after two days of conception and is unique to humans as well as other animals, can have an impact on life-long health problems. This discovery could help women with these variants live more comfortable lives by providing them opportunities for treatment options through our drug design efforts at WEHI.
To view the original scientific study click below:
Maternal SMCHD1 regulates Hox gene expression and patterning in the mouse embryo



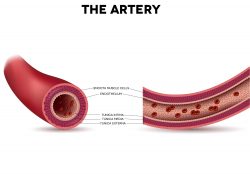 From the early 1900’s blood banks have been crucial in medical care. A team is now wanting to take the concepts a step further by utilizing stem cells in creating new arteries for people that have cardiovascular diseases. They have discovered a drug that might help decrease complications in people who undergo bypass surgery.
From the early 1900’s blood banks have been crucial in medical care. A team is now wanting to take the concepts a step further by utilizing stem cells in creating new arteries for people that have cardiovascular diseases. They have discovered a drug that might help decrease complications in people who undergo bypass surgery. A new study is trying to understand early heart disease and development in relation to the mechanisms that determine cell fate. PSCs, or human pluripotent stem cells can conceivably produce a tissue the human body needs for repair. But developing technology for this to happen for a specialized cell, for example a beating heart muscle cell, has required intricate knowledge of developmental pathways and regulatory factors.
A new study is trying to understand early heart disease and development in relation to the mechanisms that determine cell fate. PSCs, or human pluripotent stem cells can conceivably produce a tissue the human body needs for repair. But developing technology for this to happen for a specialized cell, for example a beating heart muscle cell, has required intricate knowledge of developmental pathways and regulatory factors. It is known that the intestinal lining needs to regenerate daily to be a powerful barrier to counter pathogens while allowing nutrients to be absorbed. The responsibility for this comes from the intestine’s stem cells. They need to meet a level of constant replenishment and repair. But, for this to happen, the stem cell needs to decide if the conditions of the intestine are receptive. If the stem cell makes the wrong decision or coordinates it poorly, intestinal cancer or diseases could occur.
It is known that the intestinal lining needs to regenerate daily to be a powerful barrier to counter pathogens while allowing nutrients to be absorbed. The responsibility for this comes from the intestine’s stem cells. They need to meet a level of constant replenishment and repair. But, for this to happen, the stem cell needs to decide if the conditions of the intestine are receptive. If the stem cell makes the wrong decision or coordinates it poorly, intestinal cancer or diseases could occur. The indoor environment is usually more dangerous than the outdoors, with 90% of people’s time spent indoors. Chemicals from a variety of sources such as outdoor pollutants can seep into your home and cause problems for you there too! When it comes to health risks our bodies are constantly being bombarded by new chemicals – some good (like oxygen), others bad such as viruses or bacteria which want nothing better then an opportunity to live off of us. You might be surprised to learn that we are extremely harmful traveling emission sources of chemicals, including those found in our skin and breath.
The indoor environment is usually more dangerous than the outdoors, with 90% of people’s time spent indoors. Chemicals from a variety of sources such as outdoor pollutants can seep into your home and cause problems for you there too! When it comes to health risks our bodies are constantly being bombarded by new chemicals – some good (like oxygen), others bad such as viruses or bacteria which want nothing better then an opportunity to live off of us. You might be surprised to learn that we are extremely harmful traveling emission sources of chemicals, including those found in our skin and breath. It has been found from reviewing 49 studies from 1800 weightlifters that increasing protein intake by double the amount increased strength by 9% and added about 1 lb of muscle growth. The participants worked out for 6 weeks and lifted weights at least twice per week.
It has been found from reviewing 49 studies from 1800 weightlifters that increasing protein intake by double the amount increased strength by 9% and added about 1 lb of muscle growth. The participants worked out for 6 weeks and lifted weights at least twice per week. 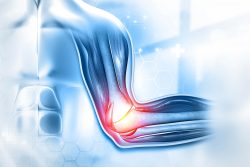 New research has identified how cells communicate to repair muscle damage. When a muscle is damaged, stem cells and immune cells work together to repair the damage. But how these cells interact to complete the removal process of dead tissue and make new muscle fibers had been a mystery. Scientists have discovered that hyaluranic acid is the essential molecule that contributes to this interaction.
New research has identified how cells communicate to repair muscle damage. When a muscle is damaged, stem cells and immune cells work together to repair the damage. But how these cells interact to complete the removal process of dead tissue and make new muscle fibers had been a mystery. Scientists have discovered that hyaluranic acid is the essential molecule that contributes to this interaction. A new study has found a way to program stem cells in order to grow new cartilage on a 3-D template of the hip joint ball. This cartilage releases anti-inflammatory molecules that assist in fending off new arthritis occurrences. The new technology could supply an alternative to traditional hip replacement surgery and could remove the need for surgery for joint replacement surgery in some people.
A new study has found a way to program stem cells in order to grow new cartilage on a 3-D template of the hip joint ball. This cartilage releases anti-inflammatory molecules that assist in fending off new arthritis occurrences. The new technology could supply an alternative to traditional hip replacement surgery and could remove the need for surgery for joint replacement surgery in some people.  Hair follicle cells divide and die. But a new study has discovered a single chemical called TGF-beta that determines when this happens. It could ultimately treat baldness and may speed wound healing. Since follicles are a stem cell source they have the unique capability to be able to turn into other types of cells. This stem cell adaptability creates a path for repair of tissues and organs that have been damaged.
Hair follicle cells divide and die. But a new study has discovered a single chemical called TGF-beta that determines when this happens. It could ultimately treat baldness and may speed wound healing. Since follicles are a stem cell source they have the unique capability to be able to turn into other types of cells. This stem cell adaptability creates a path for repair of tissues and organs that have been damaged. While we sleep there are brain circuits and neuron learning connections that are active. They help us establish differences between items that are unrelated. The ability to remember indirect or arbitrary links between people, objects or events is called relational memory. This is what helps you put names with faces, find your keys or remember to turn off the stove before you leave the house.
While we sleep there are brain circuits and neuron learning connections that are active. They help us establish differences between items that are unrelated. The ability to remember indirect or arbitrary links between people, objects or events is called relational memory. This is what helps you put names with faces, find your keys or remember to turn off the stove before you leave the house.