Anti-Inflammatory Molecules That Decline In the Aging Brain
 In aging, a lot of things happen including inflammation, stress, and changes in metabolism. A group of scientists has now found that a type of lipid called SGDGs (3-sulfogalactosyl diacylglycerols) declines in the brain as we age. These molecules may lead to the discovery of new ways to treat neurological diseases due to aging. The study helps understand the molecular basis of aging of the brain and offers new avenues of therapeutic intervention.
In aging, a lot of things happen including inflammation, stress, and changes in metabolism. A group of scientists has now found that a type of lipid called SGDGs (3-sulfogalactosyl diacylglycerols) declines in the brain as we age. These molecules may lead to the discovery of new ways to treat neurological diseases due to aging. The study helps understand the molecular basis of aging of the brain and offers new avenues of therapeutic intervention.
The study found the molecular basis of declining anti-inflammatory molecules in the aging brain may be due to processes that regulate aging. Lipids play a crucial role in this process.
The research team discovered three things involving anti-inflammatory molecules. The family members of SGDGs and associated lipids are changed substantially with the aging process. They may be guided by processes that regulate the aging process, and lipid levels are very different in older mice than younger mice. This may play an important role in the decline of anti-inflammatory molecules. This is an important discovery that should be studied further.
The researchers used liquid chromatography-mass spectrometry to study the brains of mice at five different ages. They then used advanced data analytics to find patterns in the lipid profiles that were age-related. Next, they built SGDG molecules that were then tested for biological activity. This research provides new insight into the molecular mechanisms that contribute to inflammation in the aging brain.
SGDGs are molecules that have anti-inflammatory properties. This could be indicative for neurodegenerative conditions and disorders that can involve an increase of brain inflammation.
They also discovered that SGDGs are present in primate and human brains, which suggests that SGDGs can play a crucial role in other animals besides mice. Ongoing research is needed to show if SGDGs influence human neuroinflammation.
The research team will further study how SGDGs regulate the process of aging, and the proteins that break them down and make them. This could help to uncover novel genetic activity linked with aging. The study of these significant lipids is completely open for discovery, with the understanding of the structure of them and the team’s skill to construct them in a lab.
To view the original scientific study click below:
A class of anti-inflammatory lipids decrease with aging in the central nervous system



 It’s no secret that getting older can take a toll on the body, with increased risks of heart disease, dementia and reduced immune function. But new research has uncovered evidence that aerobic exercise may combat those effects by actually reversing aging’s impact on essential muscle stem cells involved in tissue regeneration. You don’t have to settle for slowing down as years accumulate. It could be possible to bounce back from workouts or illnesses more easily than before.
It’s no secret that getting older can take a toll on the body, with increased risks of heart disease, dementia and reduced immune function. But new research has uncovered evidence that aerobic exercise may combat those effects by actually reversing aging’s impact on essential muscle stem cells involved in tissue regeneration. You don’t have to settle for slowing down as years accumulate. It could be possible to bounce back from workouts or illnesses more easily than before. Our brain is capable of generating new neurons even late in life, an ability which plays a vital role in memory processes. Unfortunately, age and Alzheimer’s can severely impede this regenerative capacity, weakening the hippocampus’ efficiency to remember.
Our brain is capable of generating new neurons even late in life, an ability which plays a vital role in memory processes. Unfortunately, age and Alzheimer’s can severely impede this regenerative capacity, weakening the hippocampus’ efficiency to remember. As we age, our bodies go through a variety of changes that can significantly affect and contribute to a decline in function. Common molecular-level transformations associated with aging include genomic instability, telomere shortening, epigenetic adaptations and mitochondrial dysfunction. Understanding these key hallmarks is an essential part of the field of aging research for those seeking successful healthy advancement into old age.
As we age, our bodies go through a variety of changes that can significantly affect and contribute to a decline in function. Common molecular-level transformations associated with aging include genomic instability, telomere shortening, epigenetic adaptations and mitochondrial dysfunction. Understanding these key hallmarks is an essential part of the field of aging research for those seeking successful healthy advancement into old age. Exercise can provide many health benefits, but a new study correlates how well our bodies respond to exercise depending on the time of day when we work out. To uncover these effects, researchers ventured to understand the relationship between biosynthesis and fat burning in relation to different times of day.
Exercise can provide many health benefits, but a new study correlates how well our bodies respond to exercise depending on the time of day when we work out. To uncover these effects, researchers ventured to understand the relationship between biosynthesis and fat burning in relation to different times of day.  Stress can prove to be more than just an emotional burden. It may also impede our bodies from properly absorbing essential nutrients. When we’re stressed, the body releases hormones that interfere with nutrient absorption in digestion. Unfortunately, this could cause many problems including fatigue and weakened immunity.
Stress can prove to be more than just an emotional burden. It may also impede our bodies from properly absorbing essential nutrients. When we’re stressed, the body releases hormones that interfere with nutrient absorption in digestion. Unfortunately, this could cause many problems including fatigue and weakened immunity. Recent studies show that transfusions of young blood hold many rejuvenating benefits for older people, such as increased heart strength and mental clarity. Many researchers are working to identify the elements in youth-filled blood so they can be replicated into a pill form. However, an even more effective approach may be found by refreshing the system within our bodies responsible for creating fresh red cells, the oxygen carriers throughout our systems. This could mean that a 70-year old with a 40 year-old’s level of new red cell production could experience extended more youthful health span, if not overall lifespan longevity.
Recent studies show that transfusions of young blood hold many rejuvenating benefits for older people, such as increased heart strength and mental clarity. Many researchers are working to identify the elements in youth-filled blood so they can be replicated into a pill form. However, an even more effective approach may be found by refreshing the system within our bodies responsible for creating fresh red cells, the oxygen carriers throughout our systems. This could mean that a 70-year old with a 40 year-old’s level of new red cell production could experience extended more youthful health span, if not overall lifespan longevity. A groundbreaking study has discovered a worrying new link between air pollution and human brain function. Utilizing Functional Magnetic Resonance Imaging (fMRI), researchers observed that even just two hours of exposure to diesel exhaust can impair the communication abilities within different areas of the brain. This may lead to decreased functional connectivity – an indicator of how well cells interact with each other in-turn affecting overall mental performance.
A groundbreaking study has discovered a worrying new link between air pollution and human brain function. Utilizing Functional Magnetic Resonance Imaging (fMRI), researchers observed that even just two hours of exposure to diesel exhaust can impair the communication abilities within different areas of the brain. This may lead to decreased functional connectivity – an indicator of how well cells interact with each other in-turn affecting overall mental performance. For more than a century, medical researchers have warned of the dangers salt poses on high blood pressure and cardiovascular deaths. But recent evidence is turning that belief upside down and suggesting it’s not salt but sugars in our diets that are driving up numbers related to heart health. A recent study published in BMJ Open Heart suggests that fructose is actually the more dangerous culprit when it comes to hypertension and heart disease.
For more than a century, medical researchers have warned of the dangers salt poses on high blood pressure and cardiovascular deaths. But recent evidence is turning that belief upside down and suggesting it’s not salt but sugars in our diets that are driving up numbers related to heart health. A recent study published in BMJ Open Heart suggests that fructose is actually the more dangerous culprit when it comes to hypertension and heart disease.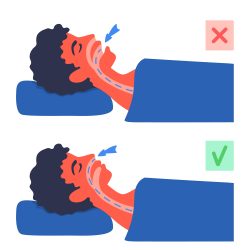 Our breath is the life source that keeps us going, and dodging any health issues related to it should be a top priority. As such, nasal breathing has increasingly gained attention as an essential element for respiratory well-being. By efficiently channeling air through your nose rather than your mouth, you are reaping numerous benefits for both short- and long-term health, whereas chronic mouth breathers may unknowingly be harmful in various ways.
Our breath is the life source that keeps us going, and dodging any health issues related to it should be a top priority. As such, nasal breathing has increasingly gained attention as an essential element for respiratory well-being. By efficiently channeling air through your nose rather than your mouth, you are reaping numerous benefits for both short- and long-term health, whereas chronic mouth breathers may unknowingly be harmful in various ways.