Successful Aging Includes Social Interaction
 A recent study tracked the health of over 7,000 middle-aged and older Canadians for three years, investigating whether increased social activity led to better long-term health outcomes. The study found that individuals who engaged in leisure activities and volunteer work were more likely to maintain excellent health and less likely to experience cognitive, physical, emotional, or mental illnesses. To qualify as successfully aging, participants had to be free of any serious conditions that hindered daily activities while also reporting high levels of happiness and good health. Only individuals who qualified at the beginning of the study were monitored to determine if social participation played a role in maintaining their excellent health.
A recent study tracked the health of over 7,000 middle-aged and older Canadians for three years, investigating whether increased social activity led to better long-term health outcomes. The study found that individuals who engaged in leisure activities and volunteer work were more likely to maintain excellent health and less likely to experience cognitive, physical, emotional, or mental illnesses. To qualify as successfully aging, participants had to be free of any serious conditions that hindered daily activities while also reporting high levels of happiness and good health. Only individuals who qualified at the beginning of the study were monitored to determine if social participation played a role in maintaining their excellent health.
Findings from the study show that engaging in volunteer or recreational activities has a significant impact on successful aging. After three years, 72% of those who participated in such activities remained were aging successfully. In contrast, only two-thirds of those who abstained from such activities were found to not age gracefully by the end of the study. These results still hold true even after adjusting for sociodemographic factors. In fact, those who engaged in volunteer or charity work were 17% more likely to maintain excellent health, while those who participated in recreational activities were 15% more likely to do so.
While the study’s observational approach precludes definitive conclusions regarding causation, a clear connection seems to exist between social activity and thriving in old age. Maintaining social connectedness is vital regardless of age. It elevates mood, decreases feelings of loneliness and isolation, and positively impacts mental and overall well-being.
As a non-pharmacological intervention, medical professionals are embracing the concept of “social prescribing” to integrate primary care with services in the community. This approach can encourage older adults to engage in volunteer work and recreational activities, thus supporting their cognitive, mental, physical, and emotional well-being as they age. These findings are significant and valuable for older adults and their families who may assume that decline is a natural part of growing old. Therefore, to secure a healthy and vibrant future for older adults, it is essential for families, healthcare providers, policymakers, and researchers to work collaboratively towards creating an enabling environment.
Ultimately, the data highlights the importance of staying active and engaged in volunteer or recreational activities for successful aging.
To view the original scientific study click below:
A Profile of Social Participation in a Nationally Representative Sample of Canadian Older Adults: Findings from the Canadian Longitudinal Study on Aging



 Recent experiments conducted at the Health and Human Performance Lab at the University of Houston have unveiled a groundbreaking discovery in the field of metabolic health. By using a muscle in your lower leg, this exercise can regulate blood sugar better than traditional methods like weight loss, diet, and low- to moderate-intensity daily exercise. Called the “soleus pushup”, this metabolism-boosting technique can be performed while sitting, making it a perfect option for those who spend a considerable amount of time sitting. Considering that the average American spends 10 hours a day in a sedentary position, this exercise is a simple yet effective way to combat the negative effects of a sedentary lifestyle.
Recent experiments conducted at the Health and Human Performance Lab at the University of Houston have unveiled a groundbreaking discovery in the field of metabolic health. By using a muscle in your lower leg, this exercise can regulate blood sugar better than traditional methods like weight loss, diet, and low- to moderate-intensity daily exercise. Called the “soleus pushup”, this metabolism-boosting technique can be performed while sitting, making it a perfect option for those who spend a considerable amount of time sitting. Considering that the average American spends 10 hours a day in a sedentary position, this exercise is a simple yet effective way to combat the negative effects of a sedentary lifestyle. Late night eating can have a significant impact on three key components of body weight regulation, including calorie intake regulation, calories burned, and molecular changes in fat tissue. Brigham and Women’s Hospital researchers have found that this can increase the risk of obesity, which affects approximately 42 percent of adults in the United States and an estimated 650 million globally.
Late night eating can have a significant impact on three key components of body weight regulation, including calorie intake regulation, calories burned, and molecular changes in fat tissue. Brigham and Women’s Hospital researchers have found that this can increase the risk of obesity, which affects approximately 42 percent of adults in the United States and an estimated 650 million globally. Recent advancements in public health and hygiene have significantly increased the average human lifespan. In the U.S., the average lifespan is currently 77 years. Although some individuals reach the impressive age of 100 years, the reasons for such exceptional longevity are not fully understood. A research team has discovered that gut bacteria may hold the key to unlocking the mystery behind long life. This groundbreaking research provides new insight into the factors that contribute to human longevity.
Recent advancements in public health and hygiene have significantly increased the average human lifespan. In the U.S., the average lifespan is currently 77 years. Although some individuals reach the impressive age of 100 years, the reasons for such exceptional longevity are not fully understood. A research team has discovered that gut bacteria may hold the key to unlocking the mystery behind long life. This groundbreaking research provides new insight into the factors that contribute to human longevity.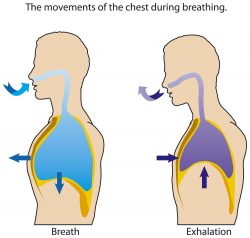 According to a recent study by scientists at Massachusetts General Hospital, increasing life span could be as simple as breathing less oxygen. While many seek to extend their lifespan through caloric restriction or exercise, this study offers an intriguing alternative. When mice were kept at oxygen levels equivalent to the base camp of Mount Everest of 11%, they lived an impressive 50 percent longer than their counterparts exposed to ambient levels.
According to a recent study by scientists at Massachusetts General Hospital, increasing life span could be as simple as breathing less oxygen. While many seek to extend their lifespan through caloric restriction or exercise, this study offers an intriguing alternative. When mice were kept at oxygen levels equivalent to the base camp of Mount Everest of 11%, they lived an impressive 50 percent longer than their counterparts exposed to ambient levels.  In recent times, a lot of emphasis has been placed on gut health. Previously underestimated, the intestinal tract is now at the forefront of attention. From fashionable products that promise to improve the gut microbiome to nutritional guidance on how to maintain healthy digestion, individuals are seeking to optimize intestinal wellbeing.
In recent times, a lot of emphasis has been placed on gut health. Previously underestimated, the intestinal tract is now at the forefront of attention. From fashionable products that promise to improve the gut microbiome to nutritional guidance on how to maintain healthy digestion, individuals are seeking to optimize intestinal wellbeing.  Alzheimer’s disease, the most prevalent form of dementia and affecting over 55 million people worldwide, is a critical global health concern. As researchers continue to work tirelessly to discover a cure for this debilitating illness, others are investigating ways to minimize the risk of developing it. While prior research has demonstrated that changes in diet and physical activity can help, a recent study has presented a groundbreaking method that shows how performing breathing exercises can lower the likelihood of developing Alzheimer’s disease.
Alzheimer’s disease, the most prevalent form of dementia and affecting over 55 million people worldwide, is a critical global health concern. As researchers continue to work tirelessly to discover a cure for this debilitating illness, others are investigating ways to minimize the risk of developing it. While prior research has demonstrated that changes in diet and physical activity can help, a recent study has presented a groundbreaking method that shows how performing breathing exercises can lower the likelihood of developing Alzheimer’s disease. As we ponder the future and what it holds, we may wonder how we can ensure a long and fulfilling life. Researchers have recently discovered that the key to healthy brain aging could lie in managing our negative emotions. By maintaining contentment and happiness, we may actually protect ourselves against the cognitive decline often associated with aging and illnesses like dementia. The latest research published in Nature Aging is an exciting step forward in understanding how we can take control of our brain health as we grow older.
As we ponder the future and what it holds, we may wonder how we can ensure a long and fulfilling life. Researchers have recently discovered that the key to healthy brain aging could lie in managing our negative emotions. By maintaining contentment and happiness, we may actually protect ourselves against the cognitive decline often associated with aging and illnesses like dementia. The latest research published in Nature Aging is an exciting step forward in understanding how we can take control of our brain health as we grow older. Napping is a widely accepted practice in regions such as Murcia, Spain, but long siestas of over 30 minutes have been linked to increased risk of obesity, metabolic syndrome and high blood pressure. According to researchers, if you’re pining for a midday snooze, make sure it’s a quick power nap. The duration, sleep posture, and other factors may have an impact on the nap’s health outcomes. To expand on this finding, the impact was investigated on metabolic health in the culturally-entrenched siesta-haven of Spain, examining the role of siesta duration. In a previous study of a large population in the UK, a like was identified between siestas and a higher risk of obesity.
Napping is a widely accepted practice in regions such as Murcia, Spain, but long siestas of over 30 minutes have been linked to increased risk of obesity, metabolic syndrome and high blood pressure. According to researchers, if you’re pining for a midday snooze, make sure it’s a quick power nap. The duration, sleep posture, and other factors may have an impact on the nap’s health outcomes. To expand on this finding, the impact was investigated on metabolic health in the culturally-entrenched siesta-haven of Spain, examining the role of siesta duration. In a previous study of a large population in the UK, a like was identified between siestas and a higher risk of obesity.  A recent study has shown that even just the sensation of hunger has the potential to slow down the ageing process. This new research, published in the scientific journal Science, reveals that the mere taste and aroma of food can, in fact, overturn the benefits of dietary restrictions. Although previous findings have established that caloric limitations can significantly boost the lifespan of animals, this latest study has found that fruit flies can increase their life expectancy through hunger alone.
A recent study has shown that even just the sensation of hunger has the potential to slow down the ageing process. This new research, published in the scientific journal Science, reveals that the mere taste and aroma of food can, in fact, overturn the benefits of dietary restrictions. Although previous findings have established that caloric limitations can significantly boost the lifespan of animals, this latest study has found that fruit flies can increase their life expectancy through hunger alone.