The Effects of Ketogenic Eating on Cellular Lifespan
 Ketogenic diets have been a very popular diet in the last few years but not without controversy and there have been no major studies on how the diet affects a person’s health. Some people use the diet to lose weight but it is also known to help manage childhood epilepsy, prohibiting neurodegenerative diseases and supporting cancer treatment. Many individuals also report feeling more energetic while experiencing other beneficial effects on the diet, although more comprehensive human studies are needed to confirm these claims.
Ketogenic diets have been a very popular diet in the last few years but not without controversy and there have been no major studies on how the diet affects a person’s health. Some people use the diet to lose weight but it is also known to help manage childhood epilepsy, prohibiting neurodegenerative diseases and supporting cancer treatment. Many individuals also report feeling more energetic while experiencing other beneficial effects on the diet, although more comprehensive human studies are needed to confirm these claims.
It is controversial in the respect that in can increase levels of LDL cholesterol, which could lead to heart disease. It has also been reported to cause bone fractures and kidney stones in adults with epilepsy. The long-term effects of this diet are not known and gives reason to reconsider this diet. A new study has investigated the diet’s effects on cellular senescence in mice using two different keto diets with interesting results.
A keto diet is high in fats, whether saturated or unsaturated. The two diets used in the study had different amounts of these fats but largely had the same results. One diet consisted of no carbohydrates, 10% protein and 90% from fats. The other diet was balanced with most of the calories from carbohydrates and some from protein and fat. The mice all consumed the same amount of calories and no substantial weight gain was noted until after 21 days, where there was a slight increase.
What was noted at the end of 21 days was an elevation of senescent cells in the heart of 15-20%. Also, there was a marked increase on cellular senescence in liver and kidney tissue. The mice displayed signs of metabolic dysregulation with higher levels of triglycerides, and LDL and HDL cholesterol. Significant levels of pro-inflammatory molecules, which can affect surrounding cells were also found.
The effects on the mice after 90 days on the keto diet were insignificant, but after 180 days showed a marked increase. This leads one to wonder what the long-term effects might be of this diet. When the mice were put back on a regular diet their senescence cells returned to normal, suggesting the damage could be reversible for a certain time period. The effects of the keto diet occurred in both younger and older mice, therefore, the diet affects all age groups the same.
The study results contend that the keto diet is intricate, manifesting both advantages and drawbacks that are influenced by a range of elements. Items as diet timing, its makeup, and the individual’s genetic profile, hormonal influences, and health status need to all be taken into consideration. Therefore, it is suggested that the starting a ketogenic diet should be evaluated and assessed to decide who might or might not see improvements from this nutritional strategy.
To view the original scientific study click below:
Ketogenic diet induces p53-dependent cellular senescence in multiple organs



 More than 60 million people globally are currently affected by Alzheimer’s disease, and projections suggest this number could rise to 78 million in the next seven years. Given these figures, it’s crucial to allocate resources towards mitigating the disease. Recent insights suggest that addressing belly fat could be a key strategy in reducing Alzheimer’s risk.
More than 60 million people globally are currently affected by Alzheimer’s disease, and projections suggest this number could rise to 78 million in the next seven years. Given these figures, it’s crucial to allocate resources towards mitigating the disease. Recent insights suggest that addressing belly fat could be a key strategy in reducing Alzheimer’s risk. A new study by the Icahn School of Medicine at Mount Sinai has uncovered a connection between poor sleep quality and serious health risks. People who consistently miss out on an hour and a half of sleep per night are more susceptible to inflammatory disorders, cardiovascular disease, as well as weakened immunity levels.
A new study by the Icahn School of Medicine at Mount Sinai has uncovered a connection between poor sleep quality and serious health risks. People who consistently miss out on an hour and a half of sleep per night are more susceptible to inflammatory disorders, cardiovascular disease, as well as weakened immunity levels. Hematopoietic stem cells (HSCs) have a remarkable longevity compared to other cells in the body. These are the cells responsible for forming blood. They produce progenitor cells that rapidly divide and generate hundreds of billions of cells each day. These cells are essential for meeting the body’s daily needs, from oxygen-transporting red blood cells and immune-defending white blood cells to clot-producing platelets.
Hematopoietic stem cells (HSCs) have a remarkable longevity compared to other cells in the body. These are the cells responsible for forming blood. They produce progenitor cells that rapidly divide and generate hundreds of billions of cells each day. These cells are essential for meeting the body’s daily needs, from oxygen-transporting red blood cells and immune-defending white blood cells to clot-producing platelets. An earphone user reported that after using AirPods for some time, he developed a persistent high-pitched tone in his ears. He has always taken great care to protect his hearing, avoiding loud noises and carrying earplugs to shield himself from potential harmful sounds. Despite these precautions, his condition worsened. He noticed that even when he inserts his AirPods and doesn’t play any audio, they emit a high-pitched tone that closely mimics his tinnitus. This experience has led him to believe that the AirPods might have caused his tinnitus.
An earphone user reported that after using AirPods for some time, he developed a persistent high-pitched tone in his ears. He has always taken great care to protect his hearing, avoiding loud noises and carrying earplugs to shield himself from potential harmful sounds. Despite these precautions, his condition worsened. He noticed that even when he inserts his AirPods and doesn’t play any audio, they emit a high-pitched tone that closely mimics his tinnitus. This experience has led him to believe that the AirPods might have caused his tinnitus. For many years, the prevailing theory was that sleep helped the brain eliminate harmful molecules. However, recent preliminary research on mice suggests this might not be the case. A new study aims to delve deeper into the reasons we need sleep, potentially challenging our initial assumptions. Findings now indicate that physical activity could be more effective than sleep in aiding the brain’s detoxification process.
For many years, the prevailing theory was that sleep helped the brain eliminate harmful molecules. However, recent preliminary research on mice suggests this might not be the case. A new study aims to delve deeper into the reasons we need sleep, potentially challenging our initial assumptions. Findings now indicate that physical activity could be more effective than sleep in aiding the brain’s detoxification process. A recent study on mice has revealed that circadian rhythms, which regulate daily physiological processes, are not solely governed by a central clock in the brain. Instead, they involve a more intricate system where molecular clocks in both the brain and muscle tissue work together to maintain muscle health and function. The research further indicates that adjusting these clocks through changes in meal timing could potentially preserve muscle function in the elderly.
A recent study on mice has revealed that circadian rhythms, which regulate daily physiological processes, are not solely governed by a central clock in the brain. Instead, they involve a more intricate system where molecular clocks in both the brain and muscle tissue work together to maintain muscle health and function. The research further indicates that adjusting these clocks through changes in meal timing could potentially preserve muscle function in the elderly. Typically, when discussing potential treatments for Alzheimer’s Disease, the focus tends to be on amyloid proteins and the plaques that form in the brain. Yet, recent studies suggest that the disease is influenced by a broader range of factors, such as neuroinflammation and metabolic imbalances. In a significant breakthrough, a team from Michigan Medicine has demonstrated that transplanting human neural stem cells into a mouse model of Alzheimer’s not only enhances memory but also diminishes neuroinflammation. This research highlights a promising new direction for therapeutic approaches.
Typically, when discussing potential treatments for Alzheimer’s Disease, the focus tends to be on amyloid proteins and the plaques that form in the brain. Yet, recent studies suggest that the disease is influenced by a broader range of factors, such as neuroinflammation and metabolic imbalances. In a significant breakthrough, a team from Michigan Medicine has demonstrated that transplanting human neural stem cells into a mouse model of Alzheimer’s not only enhances memory but also diminishes neuroinflammation. This research highlights a promising new direction for therapeutic approaches.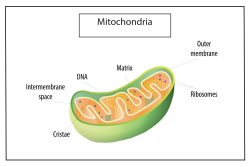 Mitochondria, often described as the powerhouses of cells, are crucial for converting nutrients into adenosine triphosphate (ATP), the energy currency of cells. Their existence is fundamental to the survival of complex organisms, including humans. However, as we age, mitochondria sustain damage and become less effective.
Mitochondria, often described as the powerhouses of cells, are crucial for converting nutrients into adenosine triphosphate (ATP), the energy currency of cells. Their existence is fundamental to the survival of complex organisms, including humans. However, as we age, mitochondria sustain damage and become less effective.  When you find yourself more alert and focused after basking in bright daylight, science offers an explanation. Recent studies reveal that exposure to increased levels of light can directly influence activity in a vital brain region, the hypothalamus, boosting cognitive performance and promoting wakefulness.
When you find yourself more alert and focused after basking in bright daylight, science offers an explanation. Recent studies reveal that exposure to increased levels of light can directly influence activity in a vital brain region, the hypothalamus, boosting cognitive performance and promoting wakefulness.