A Study led by a team of researchers at Cedars-Sinai has completed a study that may revolutionize orthopedics. They have successfully repaired severe limb fractures in laboratory animals. They used an innovative technique that signaled bones to regrow its own tissue combining an engineering approach with a biological approach for advancing regenerative engineering. Six different departments at Cedar-Sinai and researchers from Hebrew University, University of Rochester and University of California were involved in the study further demonstrating the effectiveness of utilizing a variety of diverse disciplines to further solutions to today?s medical challenges.
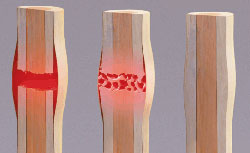
Currently more than 2 million bone grafts are performed worldwide each year due to severe injuries such as traffic accidents, war or major surgery. These injuries many times create a large gap between the edges of a fracture resulting in the inability of the bone to bridge the gap on its own. Currently pieces from a patient?s or a donor?s bone must be implanted into the gap. These bone grafts unfortunately carry disadvantages in skeletal repair. Many times healthy bones are not available for the repairs and implants that do occur can prolong pain and longer hospital stays. And some repairs fail.
The researchers devised a new technique as a possible alternative to the bone grafts. They constructed a matrix of collagen which they implanted in the space between two sides of a fractured leg bone in the animals. Collagen is a protein that the body uses to build bones. The matrix recruited the broken leg?s own stem cells into the gap over two weeks. The team delivered a bone-inducing gene directly into the stem cells to being the bone repair process. The process involved using an ultrasound pulse and micro-bubbles which facilitated the gene entry into the cells. Just eight weeks after the surgery, the bone gaps were closed and the fractured legs were healed in all lab animals used in the treatment process. Furthermore, the bone growth that occurred in the gap was as strong as surgical bone grafts.
By demonstrating that gene delivery into an animal?s own stem cells through ultra-sound was effective, the study has opened up new possibilities for treating non-healing bone fractures.
Reference: Maxim Bez1, Dmitriy Sheyn, Wafa Tawackoli, Pablo Avalos, Galina Shapiro1, Joseph C. Giaconi, Xiaoyu Da, Shiran Ben David, Jayne Gavrity, Hani A. Awad, Hyun W. Bae, Eric J. Ley, Thomas J. Kremen, Zulma Gazit, Katherine W. Ferrara, Gadi Pelled, Dan Gazit; In situ bone tissue engineering via ultrasound-mediated gene delivery to endogenous progenitor cells in mini-pigs; Science Translational Medicine, 17 May 2017: Vol. 9, Issue 390, eaal3128 DOI: 10.1126/scitranslmed.aal3128
Abstract: More than 2 million bone-grafting procedures are performed each year using autografts or allografts. However, both options carry disadvantages, and there remains a clear medical need for the development of new therapies for massive bone loss and fracture nonunions. We hypothesized that localized ultrasound-mediated, microbubble-enhanced therapeutic gene delivery to endogenous stem cells would induce efficient bone regeneration and fracture repair. To test this hypothesis, we surgically created a critical-sized bone fracture in the tibiae of Yucat?n mini-pigs, a clinically relevant large animal model. A collagen scaffold was implanted in the fracture to facilitate recruitment of endogenous mesenchymal stem/progenitor cells (MSCs) into the fracture site. Two weeks later, transcutaneous ultrasound-mediated reporter gene delivery successfully transfected 40% of cells at the fracture site, and flow cytometry showed that 80% of the transfected cells expressed MSC markers. Human bone morphogenetic protein-6 (BMP-6) plasmid DNA was delivered using ultrasound in the same animal model, leading to transient expression and secretion of BMP-6 localized to the fracture area. Micro?computed tomography and biomechanical analyses showed that ultrasound-mediated BMP-6 gene delivery led to complete radiographic and functional fracture healing in all animals 6 weeks after treatment, whereas nonunion was evident in control animals. Collectively, these findings demonstrate that ultrasound-mediated gene delivery to endogenous mesenchymal progenitor cells can effectively treat nonhealing bone fractures in large animals, thereby addressing a major orthopedic unmet need and offering new possibilities for clinical translation.





